I don't usually excerpt, so take it as a measure of my complete dismay about this.
Asymptomatic Carriers of AI Confirmed in S. Korea 2014-02-04
..The Korea Centers for Disease Control and Prevention confirmed that ten people who had participated in culling birds during the outbreaks of bird flu in 2003 and 2006 had antibodies for the H5N1 strain of avian influenza....
...The agency said that it had announced before that there were no human infection cases as asymptomatic carriers are not regarded as patients under the World Health Organization standards.
What? Seriously? You cannot be listed as a Case unless you are symptomatic?!
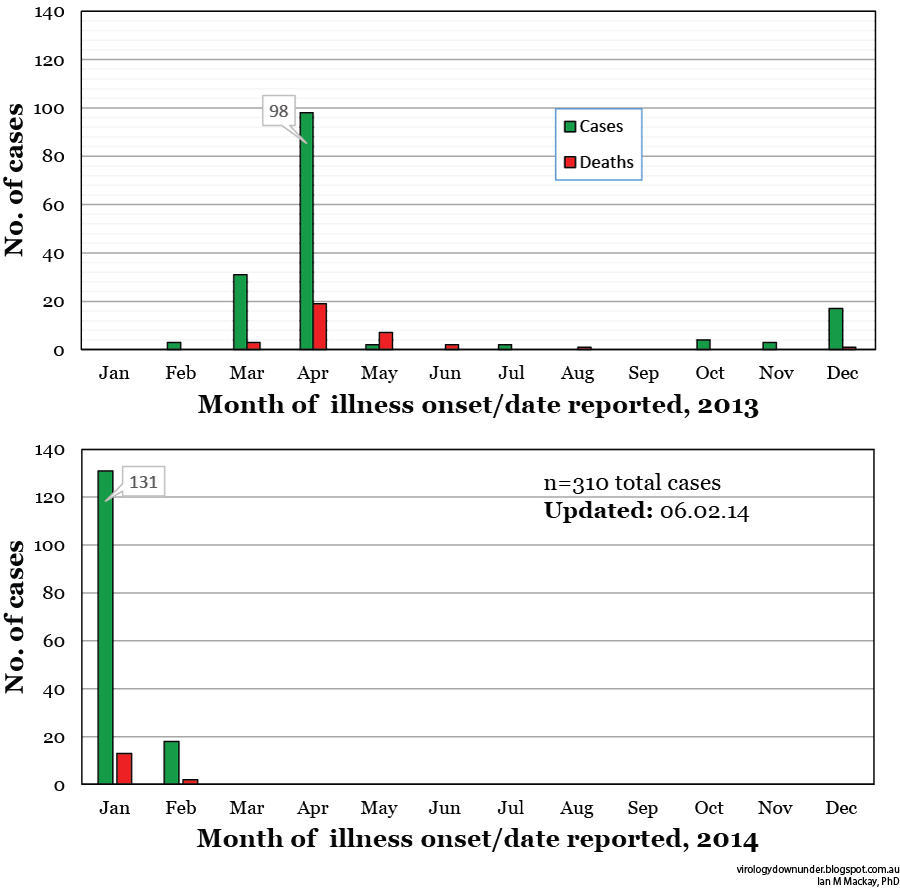
I can understand that a symptomatic Case will require medical care and resources and is a priority in counting the true human toll from an infectious agent spreading among people, but to be excluded from any Case counts when you are still a viable piece in the transmission chain puzzle (see image below)? That makes no sense to me at all. Unless there is concern that the laboratory is at fault or that the test is untrustworthy. But there are no mentions of those issues.
I've pasted below the most up-to-date H5N1 Case Definition (CD) I could locate on the World Health Organizations's (WHO) website. It's from 2006 but there does not seem to be anything more contemporary (at least on H5N1 CDs) at WHO.Confirmed H5N1 case (notify WHO)
A person meeting the criteria for a suspected or probable case
AND
One of the following positive results conducted in a national, regional or international influenza laboratory whose H5N1 test results are accepted by WHO as confirmatory:
a. Isolation of an H5N1 virus;
b. Positive H5 PCR results from tests using two different PCR targets, e.g. primers specific for influenza A and H5 HA;
c. A fourfold or greater rise in neutralization antibody titer for H5N1 based on testing of an acute serum specimen (collected 7 days or less after symptom onset) and a convalescent serum specimen. The convalescent neutralizing antibody titer must also be 1:80 or higher;
d. A microneutralization antibody titer for H5N1 of 1:80 or greater in a single serum specimen collected at day 14 or later after symptom onset and a positive result using a different serological assay, for example, a horse red blood cell haemagglutination inhibition titer of 1:160 or greater or an H5-specific western blot positive result.
So Korea's CDC had lab results (the stuff after the "AND"). What else does a person "meeting the criteria for a suspected or probable case" have to be diagnosed with for them to be a confirmed case? See the relevant section below with my highlighting (read the entire thing, in its intended order here)
Suspected H5N1 case
A person presenting with unexplained acute lower respiratory illness with fever (>38 �C ) and cough, shortness of breath or difficulty breathing.
AND
One or more of the following exposures in the 7 days prior to symptom onset:
a. Close contact (within 1 metre) with a person (e.g. caring for, speaking with, or touching) who is a suspected, probable, or confirmed H5N1 case;
b. Exposure (e.g. handling, slaughtering, defeathering, butchering, preparation for consumption) to poultry or wild birds or their remains or to environments contaminated by their faeces in an area where H5N1 infections in animals or humans have been suspected or confirmed in the last month;
c. Consumption of raw or undercooked poultry products in an area where H5N1 infections in animals or humans have been suspected or confirmed in the last month;
d. Close contact with a confirmed H5N1 infected animal other than poultry or wild birds (e.g. cat or pig);
e. Handling samples (animal or human) suspected of containing H5N1 virus in a laboratory or other setting.
Probable definition 1:A person meeting the criteria for a suspected case
AND
One of the following additional criteria:
a. infiltrates or evidence of an acute pneumonia on chest radiograph plus evidence of respiratory failure (hypoxemia, severe tachypnea)
OR
b. positive laboratory confirmation of an influenza A infection but insufficient laboratory evidence for H5N1 infection.
Probable definition 2:
A person dying of an unexplained acute respiratory illness who is considered to be epidemiologically linked by time, place, and exposure to a probable or confirmed H5N1 case.
Korea's CDC had no choice but to exclude what appear to be retrospectively confirmed, real avian influenza A(H5N1) virus cases of infection because they adhered to the letter of the CD.  |
Click on image to enlarge.
Excluding cases from official reporting & tallies
because they are asymptomatic or don't meet the
"AND" and "OR" extra criteria may make tracking
infections to their source that much more difficult. |
In doing so, they omitted reporting cases that could have held vital epidemiological information; these cases may have linked 1 severe case to another otherwise sporadic case via an asymptomatic link. The linkage might explain how a case "popped up" or it might better define person-to-person spread. They may not have done any of this too. I have no idea of the history of these 10 cases nor any of their contacts nor any H5N1 cases that may have occurred around the same time.
But the possibility exists that they could have had a role in improving understanding of the spread of a new or newly identified virus. Could this particular CD discourage more comprehensive testing of less ill groups? That would be unfortunate. There is already far too much that we don't know about the spread of influenza, let alone all the other respiratory viruses.
Take a look at the US Center for Disease Control and Prevention's CD advice for H5N1 and for H7N9; it leaves out the need for symptomatic illness in defining a confirmed case. However it does retain "illness compatible with influenza", which clearly implies a symptomatic event, as a prerequisite for a "case under investigation".
What is also very informative to this debate though, is that the WHO's much more contemporary CD for reporting MERS-CoV infection does take into account asymptomatic cases..
Asymptomatic cases: The demonstration of asymptomatic infection is useful for epidemiological investigations and should be pursued as part of case investigations, however, the burden of proof must be higher due to the risk misclassification because of false positive tests due to laboratory contamination. Generally, in most viral infections, an immunological response such as development of specific antibodies would be expected even with mild or asymptomatic infection and as such serological testing may be useful as additional confirmation of the diagnosis. Additional steps to reconfirm asymptomatic cases, or any case in which the diagnosis is suspect, could include re-extraction of RNA from the original clinical specimen and testing for different virus target genes, ideally in an independent laboratory.
This may mean that the H5N1 definition was just out of date and is in dire need of modernisation.
One implication from the Korean statement, to my mind at least, is that an absence of symptoms has been taken to mean an absence of importance in the chain of transmission because that person was not registered as a Case. I suspect that the simple act of listing a person carries significant weight. I just can't see how leaving even 1 lab-confirmed but asymptomatic person off such a list benefits the search for an answer to how an emerging virus is spreads. At least, I haven't read a convincing case for any such benefit (pun intended).
[UPDATE] Reply from WHO's Gregory H�rtl (@HaertlG)