|
The bar along the top depict how much time passed between each 100 cases.
Click on chart to enlarge. |
For a virus that is chugging along without the aid of any new genetic changes, and perhaps showing up more often (a) because of enhanced testing and/or (b) because of a large-scale breakdown in infection prevention and control (IPC), this curve sure does depict the possibility that we had no idea how much MERS-CoV was transmitting among the population. Still a poor transmitter compared to an influenzavirus, because we have seen a few larger MERS-CoV studies than show few to no MERS-CoV positives, but still more people positive than we thought.
Can we really lay this rate of climb at the feet of poor IPC alone? Wouldn't that also mean that every other respiratory virus would do this too? Perhaps not if MERS-CoV was the only one capable of causing acute pneumonia. It isn't. So shouldn't all hospitals always be full of acute pneumonia and respiratory disease among older males with comorbidities? These are modern hospitals after all. Also modern doctors with great training and skills acquired from all over the world. Perhaps poor IPC plus enhanced testing is an option? Maybe. Probably most likely when combined with an outbreak that starts in April for an unknown reason.
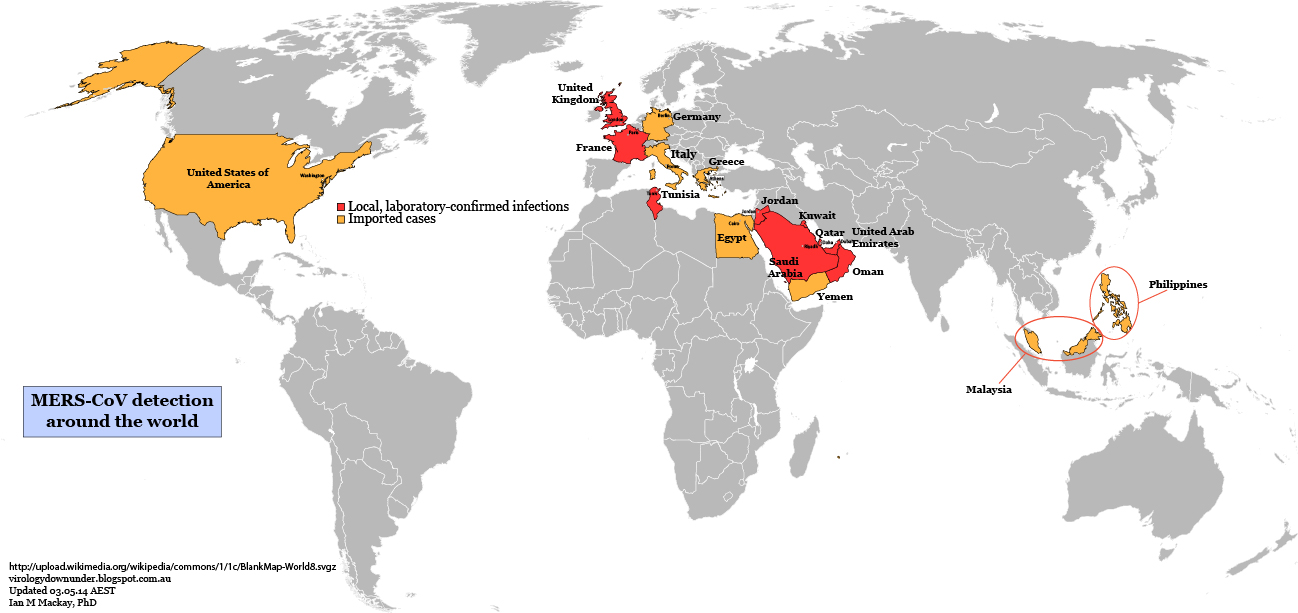
What about this option, which focusses on testing alone? Better levels of testing are at last showing it like it really is in the Arabian peninsula? This options proposes that we've been underestimating the ability of MERS-CoV to travel from person-to-person, all along. An underestimation driven by testing only the "tip of the iceberg" of disease and just watching the rest of the iceberg from a distance? What if severe disease is only found in already ill older males and most (granted, not all) of the rest get milder or unnoticeable disease but do get infected? Yes, in the past 2 weeks 5,000 samples have been tested in the Kingdom of Saudi Arabia (KSA) to yield ~140 MERS-CoV detections (~3%). After the 2012 Hajj, 154 pilgrims were tested by Gautret et al and, despite a high proportion with respiratory symptoms (83%), none were found positive for MERS-CoV. At 3% in Jeddah, testing of the Hajjis should have yielded ~4 detections among this cohort if the distribution of MERS-CoV was at this level all the time. In screening 5,065 cases and their contacts (family and healthcare workers) over a year from 1st-Oct-2012, Memish et al reported 106 detections (~2%) and no significant rise in case detection rates over that year. So a very similar proportion of positive cases, and both Jeddah and this larger study have similar numbers and a roughly similarly broad population being tested. Of course, even endemic human CoVs are not always detectable every year at the same site. Some have a biennial periodicity.
So perhaps 2-3% prevalence, similar to endemic CoVs, is the magic number for MERS-CoV positivity? Which just leaves the question, why weren't more Hajjis positive last year? Or was that just a testing thing too?
Just wondering out loud here.