Update #1 18JUN2015
 |
| Jayme and colleagues find some "smoking bats"-possible bat reservoir species for Reston ebolavirus in the Philippines. |
In what I think is only the second example of this, a new collaborative study from Jayme and a team of eminent researchers in the Philippines, Australia, Vietnam and the United States, have reported the finding of Reston ebolavirus (RESTV) viral RNA and antibodies to viral infection in a range of different bat species....some more "smoking bats" - bats with more than just past evidence, sometimes considered vague and unreliable, of an ebolavirus being hosted by the animal.
The finding of RNA is not the same as actual infectious virus, but RNA is a very specific marker for the virus nonetheless. And the authors note that they didn't want to kill the bats so only a small volume of sample was available-not enough for culture.
Leroy and colleagues had previously reported finding Zaire ebolavirus RNA and antibodies against this species of virus in Hypsignathus monstrosus, Epomops franqueti and Myonycteris torquatebats, all fruit-eating megabats of the family Pteropodidae. These are considered to be important reservoir hosts, yet they do not show signs of disease.[2]
According to one of the authors on the latest study, bats in the Philippines also seemed clinically well...
@MackayIM all bats we sampled appeared clinically healthy.� Jonathan Epstein (@EpsteinJon) July 17, 2015
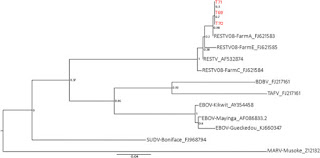 |
| Locating the Philippine RESTV sequences on the ebolavirus phylogenetic tree. Jayme et al. Virology J. (2105) 12:107.[1] |
Jayme's findings are important to the story of RESTV importations to animal facilities in the United States from the Philippines which occurred multiple times between 1989 to 1996. These fed into the dramatized retelling we know of as The Hot Zone. There were also signs of antibodies to the virus in humans working with infected non human primates in the Philippines in 1994, 1996 and 2008.
The amount of viral RNA in most of the bats was quite low - but was usually repeatably detectable. I'm a firm believer in PCR giving a specific signal when there is something specific present to detect (assuming it was done in a professional laboratory setting that reduces the risk of false positives-which it was in this instance). So low viral loads are not no viral loads.
RESTV RNA was repeatably found in oropharyngeal swabs taken from bats assigned to the following species:
- Cynopterus brachyotis (Lesser dog-faced fruit bat; range; fruit bat)
- Miniopterus australis (Little long-fingered or little bent-wing bat; range; insectivorous bat)
- Miniopterus schreibersii (Schreiber's Bent-winged Bat; range; insectivorous bat)
...and in one sample from:
- Chaerephon plicata (Wrinkle-lipped Free-tailed Bat; range; insectivorous bats)
Jayme and colleagues also sampled the blood of 61 flying foxes (of the fruit-eating bat family Pteropodidae) and antibodies were found by ELISA and Western blot in 3 Acerodon jubatus (giant golden crowned flying fox; range) bats and by ELISA alone in a Pteropus vampyrus (Large flying fox; range). If you trust the test, then this indicates past exposure.
Superman and the Joker know very well - Bats can be very tricky. But at least this finding helps to further address the Riddle(r) of the reservoir. Now, if only we could only nail down the specific culprit(s) in West Africa.
References...
- Molecular evidence of Ebola Reston virus infection in Philippine bats
- Fruit bats as reservoirs of Ebola virus
- Many details about bats to be found at the excellent IUCN Red List
http://www.iucnredlist.org/ - Population Structure of a Cave-Dwelling Bat, Miniopterus schreibersii: Does It Reflect History and Social Organization?
http://jhered.oxfordjournals.org/content/100/5/533.full - Seasonal movements of the Schreibers� bat, Miniopterus schreibersii, in the northern Iberian Peninsulahttp://www.tandfonline.com/doi/abs/10.1080/11250000801927850#.Vamrtvnzp1M
- Added bat specie range data (and discussion) from IUCN Red List and Wikipedia.







